
1 Tantalum coating
Tantalum is coated on the surface of some medical metals with its excellent corrosion resistance to prevent the release of metal elements and improve the biocompatibility of metals.
Balla prepared porous tantalum coating composites by depositing tantalum powder on the surface of titanium substrate using laser engineered net forming technology (LENSTN). The porosity is 45% - 73%, and the elastic modulus is 2 - 20Gpa. Porous tantalum coating has higher surface energy and hydrophilicity than porous titanium coating, and HOB has higher adhesion and proliferation ability at early stage on its surface. The composite combines the excellent biocompatibility of tantalum and the good mechanical properties of titanium, overcoming the defects of high cost and technical difficulty of pure tantalum.

In addition, LENSTN technology can fully melt tantalum powder, resulting in higher fatigue strength of implants. Tang et al. used vacuum plasma spraying technology to form porous tantalum coating on the titanium surface. In vitro experiments found that the coated titanium had good biocompatibility and bone induction activity. In vivo experiments in rabbits showed that it effectively improved bone formation.
2 Tantalum nanotubes
Nanotubes have attracted much attention due to their unique physical and chemical properties, and become a new hotspot in the field of nano science. Research shows that TiO2 nanotubes can promote osteoblast adhesion, proliferation and differentiation, and show a strong bone binding ability.
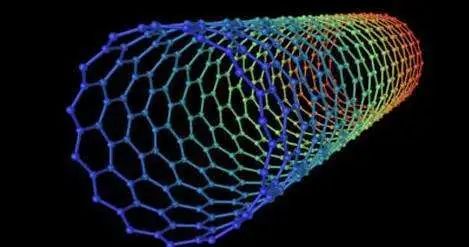
UCKH et al. prepared Ta2O5 nanotubes with HF and H2SO4 as electrolyte by anodic oxidation method. In vitro, it significantly enhanced the adhesion, proliferation and differentiation of human osteoblasts. Wan g et al. treated tantalum with anodic oxidation method, and then heated at 500 ℃ for 2h to obtain tantalum nanotubes. The study found that tantalum rice tubes have good corrosion resistance, can adsorb proteins and promote the adhesion, proliferation and differentiation of stem cells, indicating that the nanotubes have entered into the biocompatibility and bone induction of tantalum, providing a theoretical basis for the application of tantalum nanotube implants. Arnold et al. used Ta (OBu) 5 as raw material to form Ti-O-Ta sol and gel on the titanium surface by the sol gel coating method. Tantalum nanotubes were obtained by drying at 100 ℃ for 24h. In vitro experiments showed that it promoted the formation of HA and enhanced the osteoinductive ability.
3 Tantalum alloy
With the development of casting technology, titanium, niobium, zirconium and other elements are added to form tantalum alloys, which maintain the corrosion resistance and mechanical properties of tantalum, simplify the preparation process and reduce the cost.

Huang et al. developed a medical titanium niobium tantalum zirconium biological alloy, and sintered pure Ti, Nb, Ta and Zr powders with mass ratio using spark plasma sintering technology. The sintering temperature is 950 ℃ - 1150 ℃, and the vacuum degree is 2Pa. The alloy has uniform structure, high density of more than 98%, elastic modulus of 41 - 50GPa, and good mechanical compatibility.
Lian et al. prepared a new type of medical titanium alloy Ti-25Nb-10Ta-1Zr-0.2Fe by vacuum consumable arc melting. The addition of proper amount of Fe and Zr elements inhibited ω The elastic modulus of the alloy is effectively reduced by the generation of phase. Cheng et al. smelt Ti35Nb3Zr2Ta alloy in a non consumable vacuum arc furnace, with an elastic modulus of 48GPa and an ultimate tensile strength of 880MP, which has a higher surface roughness and better hydrophilicity than Ti6Al4V. Rat osteoblasts are superior to Ti6Al4V in adhesion, extension, proliferation and differentiation, showing good biocompatibility, which is expected to become a new artificial tooth implant material.
4 Porous tantalum implant administration
Implantable sustained-release drug delivery has always been a research hotspot in the field of biomedicine. Professor Liu Hongchen, based on a large number of basic and clinical studies, proposed the drug delivery theory of artificial dental implants. Loading drugs on dental implants and releasing them to the surrounding bone tissue can make the drugs play a role locally, efficiently and continuously, thus enhancing the bone integration ability of implants and reducing adverse reactions caused by systemic drug administration.
The micro pore morphology on the surface of dental implants not only promotes the formation of good bone bonding with bone tissue, but also facilitates the adhesion of various macromolecular drugs, cytokines, etc., showing its great potential in drug loading. Tantalum nanotube is a good drug carrier, which can control the degradation of bioactive molecules. It is an effective way to solve the initial stability of dental implants and long-term biological osseointegration.
5 Outlook
Porous tantalum has the advantages of low elastic modulus, high friction coefficient, and good biocompatibility. As a dental implant material, it shows a broad development prospect. The rapid development of tantalum processing technology also creates conditions for the research and development of tantalum artificial dental implants.
Although the research on tantalum artificial teeth and dental implants started late, many studies are still in the basic stage, and its clinical application effect remains to be verified and considered by multi center evidence-based medicine. How to deal with the complex oral flora environment is also the challenge of its success rate. Dental implant assisted drug delivery is also the trend of future development. Porous tantalum pore structure facilitates drug loading, which is conducive to improving the initial stability of implant repair with systemic chronic diseases and biological bone bonding. With the development of research, porous tantalum dental implants are expected to replace titanium as a new generation of dental implant materials.